
Free initial consultation
Click here to find out if you are eligible.
Check eligibility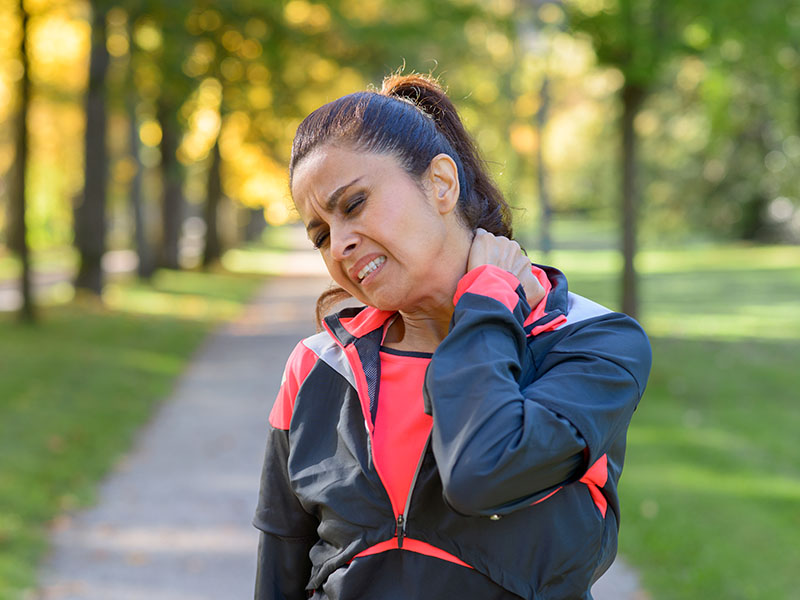
The Patient’s Story – Jessica is a 51-year-old Mum with a large family and a very physically active lifestyle that became affected by chronic pain in her neck, resulting from a skiing accident a few years before.
In 2017 I had gone skiing with my family in Switzerland. We are family of good skiers, but as my boys grew older, they soon surpassed my skill and speed level and on the day of my fall, after a lunch on the slopes, they persuaded me to go out on an afternoon ski with them and my husband. Knowing how fiercely competitive they all are I made them promise not to race off and leave me behind. Of course, predictably this is exactly what happened! I tried to catch up with them, going much faster than I was comfortable with.
Taking a corner, I hit some ice and had a wipe-out fall. I remember at the time my neck flicking backwards and really smacking my head on the ice. I lay there for a minute terrified that I had broken something. I was literally seeing stars and my ears were ringing. In the ridiculous way that you do when you fall, I pulled myself up as soon as I could, desperate to find out if I was still in one piece and I could move everything. I was helped to the side of the slope by a friendly skier who had been kind enough to stop. I spent ten minutes collecting myself before attempting to limp down the mountain, until I came across my husband, who had turned back to find me.
That was the end of my skiing for the week and my neck was stiff and painful but by the time I returned to the UK, I felt pretty much normal and carried on with life as usual for the next six months or so.
I then started to become aware of a deep aching pain in my neck that just would not go away. The pain crept down my neck and into my left shoulder and arm. At the time I didn’t know It, but this was nerve pain that would eventually wake every night bang on 2 AM!
Initially the pain would come and go, and I would dose up on over-the-counter painkillers, but over time I found that it was limiting the amount of exercise I was able to do. It also made me extremely grumpy and generally out of sorts. My sleep at night was very disturbed as I had pain down my left side and could not get comfortable. It led to me feeling low and miserable and hugely affected me enjoying time with my family, as all I really wanted to do was go and lie on my bed. When you are suffering chronic pain, it affects the whole family unit as you just aren’t yourself and it’s hard to feel excited or show interest/get involved with your kids when you feel constant pain. It’s like your attention is somewhere else the whole time.
It was when my husband pointed out the dangerously high number of empty painkiller boxes, that were appearing in the bathroom bin that I had to address the situation. I made an appointment with a top London spine surgeon and had a brain scan and 2 different types of MRI of different cross sections of my neck and back. My husband came with me to meet with the surgeon and go through the results, as I was feeling very nervous about what was wrong with me by this point.
What the images clearly showed was that my C4, C5 and partially my C6 cervical disks showed major degeneration, were bulging and pretty much touching the spinal cord. Typically, this type of injury can take some time to start hurting, after the initial impact, so it came as no surprise to the consultant that my fall had taken place six months before. My doctor presented me with a range of options – I was a candidate for an operation called an ACDF ( anterior cervical discectomy and fusion) – this involves slicing open the front of your neck to access the spine, removing the damaged disks and replacing them with artificial ones that are held in place by a titanium cage. Whilst generally successful and relatively commonly conducted on professional sportsmen, especially rugby players! There is risk to your vocal cords and obviously every operation involving the spinal cord is a big deal. The recouperation time from the op was also a consideration. Before I took this route, he recommended that I try a course of transforaminal epidural steroids. I did this for about 6 months until the specialist that I was seeing refused to inject me anymore and said there there was no point as further injections would not help and advised that I went ahead with the operation. These injections were a pain as I was sedated first and had to spend a day in hospital every few months and I had horrible brain fog from the anaesthetic for a day or two afterwards. I did see a specialist consultant physiotherapist but any manipulation or pressure upon the area actually just made the pain worse. It was at this point I tried cannabis, really as a last attempt to find a solution before undergoing the operarion.
Getting your cannabis medicine treatment right takes a while and for me it was a balancing act of getting the correct percentage of THC and CBD in an oil, specially mixed for me and then vaping an Indica flower at night and if additional pain relief was needed in the day a sativa blend. Though this became unnecessary once I was taking the oil 3 times a day. Getting to this point, I went “Low and Slow” in the trial-and-error process – the catchphrase of Integro Medical Cannabis Clinics.
I have now reached a “sweet point” in terms of my dosage, which I feel it just right and I am living pain free at the moment. I am able to run, weight train and do yoga again and feel in peak fitness. But I do listen to my body and never over do things and check in with Integro every couple of weeks.They are absolute expert on all thing’s medicinal cannabis, having been an advocate for years and lived with a partner who uses it to control his chronic Crones condition successfully.
I’m very much a cannabis evangelist these days and happy to speak to anyone who has reservations or worries about the bad reputation cannabis has. Cannabis is simply an amazing pain medicine that can make a tremendous difference to your quality of life and has none of downsides of traditional pain medicines such as addiction, brain fog and constipation.